
Preventive treatment at risk of attack
The regenerative medicine has taken a new scientific step forward, which we explain in this post.
The deposition of cholesterol plaques that leads to clogging of the coronary arteries is called atherosclerosis..
Atherosclerosis can lead to serious problems such as heart attacks, strokes and even death.
The existing treatment for patients with clogged arteries is the angioplastywhich is used to remove the material causing the blockage. The problem is that the blockage often recurs.
Angioplasty " also called percutaneous coronary intervention (PCI) " is a method by which the physician threads a deflated balloon or balloon on a catheter from the femoral artery or the radial inguinal artery through the blood vessels until they reach the site of the blockage in the heart. At the blockage, the balloon is inflated to open the artery, allowing blood to flow. A stent is often placed at the blockage site to permanently open the artery.
The bypass surgeryCoronary artery bypass surgery, in which blood vessels are used to bypass the blocked region, is often successful. In coronary artery bypass surgery, arteries or veins from another part of the patient's body are grafted into the coronary arteries to bypass the narrowing caused by atherosclerosis, allowing blood to flow around the blocked or narrowed coronary artery. Because it requires open heart surgery, it is reserved for cases of multiple narrowing of the coronary arteries..
However, researchers at the Stanford University in California have conducted a study that could lead to a therapy that induces heart cells to form new arteries.
A radical new treatment for heart disease could be developed after these scientists have found cells that can grow in fresh arteries and restore blood supply to the organ.
The work paves the way for natural bypass therapies that induce heart cells to form new arteries capable of re-routing blood around blocked and diseased blood vessels.
Patients may undergo this treatment after a heart attack, or as a precautionary measure. if they are at risk, to provide them with additional arteries that would be ready to relieve themselves in the event of blockage.
"Whenever we have a blockage in a coronary artery, the blood supply is interrupted, and you need a new supply," he said. Kristy Red-Horsewho led the research with Katharina Volz at Stanford University in California. "We want to induce, to persuade, the arteries to form and grow around the blocked area.
In patients with coronary artery disease, the arteries that supply the heart with oxygen-rich blood are narrowed by the build-up of fatty tissues. In some, this narrowing forces blood into a smaller network of neighbouring vessels, which changes the blood flow around the diseased artery.
But these collateral blood vessels are not large enough to supply the heart with all the blood it needs. What the Red-Horse researcher hopes to achieve is to grow fully capacitated arteries that can be relieved when a heart attack occurs.
"What we really need to know is how to make these large arteries to allow a lot of new blood to flow and get to the heart," he said.
Until now, one of the main obstacles to such a therapy has been scientists' lack of understanding of how coronary arteries are formed. In particular, it was not clear which cells in the heart form smooth muscle sheaths needed to create new arteries, and whether they existed in adults.
In the eLife magazinethe Stanford team describes how they tracked the cells that form arterial muscle in adult mice. They started with the addition of a fluorescent label to a single cell in the epicardiumthe layer of tissue that lines the heart.
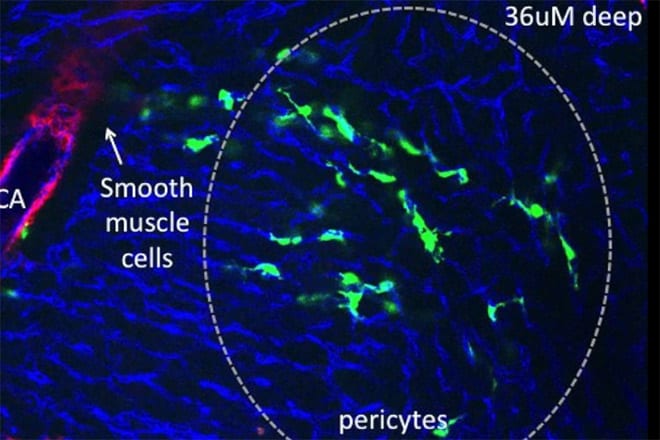
The tag allowed scientists to trace the epicardial cell and all the generations of cells it gave rise to as it divided.. The researchers noticed that some of the cells went on to become arterial muscle cells. Working from these, they identified the cells that give rise to arterial muscle, called pericytes..
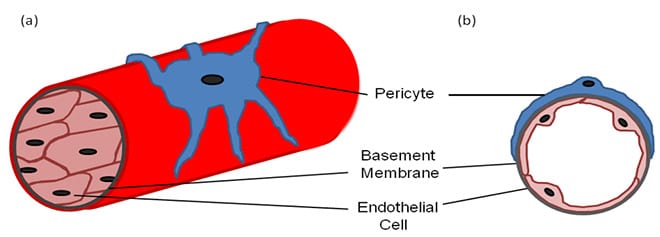
In other tests, the team exercised the molecular signals that tell pericytes to grow into arterial muscle cells. If the signals can be mimicked or mimicked by a drug, then heart cells could potentially be persuaded to form fresh arteries. on the surface of the heart, through which blood can flow.
The team has not yet done studies on the human heart, but shared physiology with the mouse heart makes them confident that the findings could help people.. Red-Horse expects to focus on growing new arteries in mice over the next five years.
There is a serious need for new treatments for heart disease and heart attacks. Of the people who suffer heart attacks each year, one in three die before they reach hospital.
Scientists like Red-Horse believe that regenerative arteries may work better than bypass surgery.
By demonstrating that pericytes are triggered to differentiate into smooth muscle cells in the developing heart, the Stanford group has reinforced the possibility that the same process can be replicated in the adult heart. The pericytes could then be used to develop new blood vessels needed to successfully repair damage after a heart attack.


0 thoughts on “Medicina regenerativa del corazón”
I am 65 years old and three and a half weeks ago I suffered an acute myocardial infarction, with extensive damage, according to my cardiologist. My heart was left with a 35 to 40% functional. My question is, how long after the infarction can the heart be treated with stem cells to try to recover some of the dead tissue, and how much would the cost of this procedure be?