3 genetic markers detect early stage patients
A panel of three genetic markers can help identify patients with early-stage lung cancer who have a very high chance of their disease returning after surgery, according to the results of a study by researchers at the US National Cancer Institute (NCI).
In the retrospective study, patients with stage I lung cancer (adenocarcinoma) whose tumours expressed all three markers were significantly more likely to die The results of the study showed that patients with tumours that did not express these markers were more likely to develop cancer or have a recurrence than patients with tumours that did not express these markers.
Post-surgical, or adjuvantChemotherapy is currently not recommended for most patients with stage I lung cancer.as it has not been shown to improve survival. However, the three-marker panelthe study authors suggested, may target a subgroup of high-risk patients who would be more likely to benefit from it.
The findings were published on 24 June in the Journal of Thoracic Oncology.
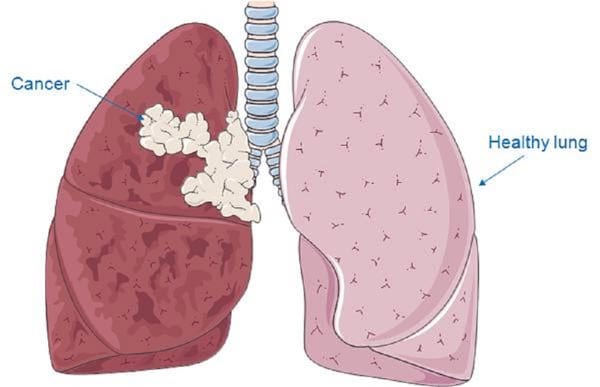
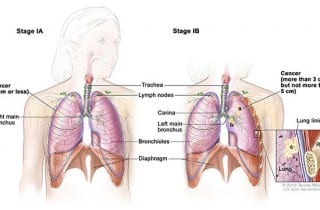
In patients with stage I disease, tumours are present only in the lungs and can often be removed surgically. However, in up to 30 percent of patients, the cancer returns after surgery and they die of the disease within 5 years.
Currently, there is no proven way to identify which of these patients have a higher risk of the disease returning, said the study's lead author, Curt Harris, M.D., of NCI's Cancer Research Center (CRC). This study is the latest in a series from Dr. Harris' lab investigating whether the different biomarkers they have identified might be able to fill this gap.
The studies, he explained, are "part of a precision medicine effort to integrate different" omics "into a single platform and develop a classifier for diagnosis and prognosis in patients with stage I lung cancer".
For this most recent study, researchers first analysed tumour and nearby lung tissue samples from patients with stage I lung adenocarcinoma who had been treated at hospitals in the Baltimore area and at centres in Norway and Japan.
Identified a specific epigenetic change in the Hoxa9 genei.e. a chemical change in the DNA, but not an alteration of the DNA sequence - called hypermethylation - that is associated with death from lung cancer within 5 years.
The researchers confirmed the association between Hoxa9 methylation status and outcome in two additional units of stage I lung cancer patients from Japan and the United States and Europe, respectively. Recurrence-free survival data were only available for these additional units, but patients with stage I disease with recurrent cancers have an extremely high risk of dying of the disease within 1 year of recurrence, said the study's lead author, Ana Robles, Ph. D., also of CRC.
In their earlier studies, Dr. Harris's team had identified two other genetic markers-overexpression of microRNA-21 and expression of four genes (XPO1, BRCA1, HIF1alpha, and DLC1). -which was also independently correlated with poor 5-year survival in patients with stage I lung cancer.
So, Dr Robles explained, they combined the three markers into a single classifier and analysed their association with outcomes in Japanese and NCI/Norway units. The classifier "produces a simple score," she continued, based on the number of markers expressed by a tumour sample.
The higher the score, they found, the higher the risk of lung cancer death or recurrence.
In the combined NCI/Norway unit, for example, patients who had received no post-surgical chemotherapy and whose tumours were positive for one, two or all three markers had a 2-, 5-, and 43-fold increased risk of lung cancer death over 5 years, respectively.
Accurate prognostic test for patients with stage I disease would have important clinical implicationssaid Dr. Robles. Based on the recent decision of the Centers for Medicare and Medicaid Services to cover the cancer screening In the case of low-dose computed tomography (CT) lung cancer in high-risk patients, its use is already growing. As a consequence, he explained, "many stage I cancers are going to be diagnosed".
Dr Harris's lab is developing an assay incorporating all three markers that can be used in prospective validation studies, he explained. They have also initiated discussions with diagnostic companies to further develop the test for potential clinical use.
Source: National Cancer Institute

