Diet in Crohn's disease
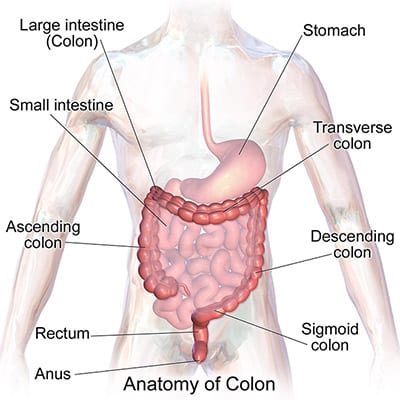
Crohn's disease is an idiopathic (of unknown cause) chronic inflammatory bowel disease, and involves any region of the gastrointestinal tract from the mouth to the anus. Swelling and inflammation can occur deep in the lining of the intestine. This can be very painful and may cause diarrhoea, abdominal pain, nausea and loss of appetite. The inflammatory process tends to be eccentric and segmental, often with normal areas of bowel between the inflamed areas.
The complications of Crohn's disease, which is one of the most common autoimmune diseasesThese include: bowel obstruction; sores and ulcers in the affected area or surrounding tissues, such as the bladder; tunnels around the anus and rectum, called fistulas; nutritional deficiencies; anaemia; arthritis; skin problems; kidney stones, gallstones or other diseases of the liver and biliary system.
Both men and women can have Crohn's disease. It can also run in families. About 20 percent (1 in 5) of people with Crohn's disease have a blood relative who has some form of inflammatory bowel disease, usually a brother or sister, and sometimes a parent.
Crohn's disease is usually diagnosed in people between the ages of 20 and 30. And about 25 percent of new diagnoses of Crohn's disease are made in people who are younger than 20 years old.
When given proper medical care, most people who have Crohn's disease are able to lead long and productive lives. New medicines and research into the causes of Crohn's disease are helping to increase the quality of life for people who have Crohn's disease.
With regard to the dietYou've probably read about different types of diets for Crohn's disease on the Internet. But the fact is that no scientifically proven diet for inflammatory bowel disease. Most experts believe, however, that some patients can identify the specific foods that trigger their gastrointestinal symptoms, especially during outbreaks of the disease. By avoiding trigger foods, your gastrointestinal symptoms of gas, bloating, abdominal pain, cramps and diarrhoea may become more manageable. At the same time, you will give your inflamed gut time to heal.
If you have had problems absorbing nutrients due to Crohn's disease, it is important to follow a high-calorie, high-protein diet, even when you don't feel like eating. In this context, the Crohn's disease diet plan, based on expert recommendations, would emphasise eating regular meals - plus an additional two or three snacks - every day. That will help make sure you get enough protein, calories and nutrients. In addition, you'll need to take your doctor-recommended vitamin and mineral supplements. By doing so, you'll be able to replenish the nutrients your body needs.
The foods that trigger symptoms are different for each person with Crohn's disease. To know which foods to leave out of your diet plan, you will need to determine which foods trigger yours. Many people with Crohn's disease find that one or more of the foods listed below aggravate symptoms during flare-ups. It is possible that at least one of these foods may trigger your symptoms:
- alcohol (mixed drinks, beer, wine)
- butter, mayonnaise, margarine, oils
- carbonated beverages
- coffee, tea, chocolate
- corn husks
- dairy products (if lactose intolerant)
- fatty (fried) foods
- foods rich in fibre
- gas-producing foods (lentils, beans, pulses, cabbage, broccoli, onions)
- nuts and seeds (peanut butter, other nut butters)
- raw fruit
- raw vegetables
- red meat and pork
- spicy foods
- whole grains and bran

Once you have identified the foods that cause you to break out, you can avoid them or prepare them differently. To do that you have to experiment with different foods and preparation methods to see what works best for you. For example, if certain raw vegetables trigger an outbreak, you don't necessarily have to give them up. You may find that steamed, boiled, or stewed you can eat that vegetable without increased gastrointestinal symptoms. If red meat increases your fat in the stool, you might try eating sirloin steak to see if you can tolerate a lean cut of beef. Or you may decide to rely on low-fat, skinless poultry and fish as your main sources of protein.
Is a low-residue diet a good diet for the treatment of Crohn's disease?
A low-residue diet is a diet in which specific foods that add waste to the stool are lowered. Many people with Crohn's disease of the small intestine have a narrowing or stricture of the lower small intestine (ileum). For these people, a low-residue diet can help reduce abdominal pain, cramping and diarrhoea. This diet may also help decrease the frequency of bowel movements for some people. Foods to avoid on a low-residue diet may include:
- corn husks
- walnuts
- raw fruit
- seeds
- vegetables
What else is important in the Crohn's disease diet?
Limiting certain foods that trigger flare-ups can help you control your symptoms, but it should not be so limited that you become malnourished. Find other sources to replace the calories, protein, carbohydrates and fats found in the foods you cut out. To do that, you must include nutrient-rich foods in your diet.
While fast foods should normally be avoided in a healthy diet, they can sometimes give your diet a needed boost. Some fast foods can offer a valuable supply of key nutrients and calories. For example, pizza offers calories, protein and nutrients such as calcium and vitamins A, B, C and D.
With regard to the liquid dietsSome research suggests that liquid diets may help people with certain health conditions, and there is evidence that some people with Crohn's disease may benefit from a high-calorie liquid diet, especially during a flare-up. By giving the intestines a well-deserved rest, the liquid diet can help suppress the symptoms of Crohn's disease. In addition, the liquid diet or special high-calorie liquid formulas may help people with Crohn's disease who need additional short-term nutrition or those whose intestines cannot absorb adequate nutrition from whole foods.

